Junctional Hemorrhage: The next frontier for hemorrhage control
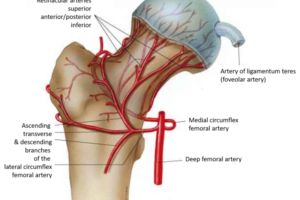
The term “junctional hemorrhage” refers to injuries and bleeding occurring at the transition zones between the extremities and the torso.
🕖 Reading Time, 4 minutes
The term first appeared in the medical literature in December 2009.
Although not an extremity, the neck is generally included in this category. Junctional hemorrhage injuries are difficult to manage as the vasculature is not amenable to circumferential compression like limb bleeding and tourniquet placement.
Prevalence of junctional wounds
19.2% of the potentially survivable battlefield deaths from Iraq and Afghanistan 2001 to 2011 involved junctional hemorrhage injuries. The groin was the most common type of junctional hemorrhage in recent combat.*1
We have no data on how often these injuries happen in civilian trauma. The Nation Trauma Data Bank records trauma patient injuries within the US, but does not use the term “junctional injury.” Rather it specifically identifies the named vascular structure injured, i.e. femoral artery, vein, etc.
Application of medical literature to civilian trauma
Extrapolating the military Global War on Terror (GWOT) prevalence to civilian trauma patients, even in active violent incidents is problematic. This is because the majority of GWOT junctional hemorrhage injuries result from IEDs. Boston notwithstanding, IED injuries are still rare in the US. Additionally, if the casualty is armored, his fatal injuries are statistically more likely to occur in non-armored areas of his body which necessarily includes junctional injuries as these are hinge points to allow for movement. The injury profile would be different in non-armored casualties.
A more applicable study to civilian trauma
Because of all of these limitations in the literature, I prefer to reference a study published by a Lebanese vascular surgeon citing his experience caring for 3000 casualties during a 13 year period during the multiple riots, civil war, and factional battles in Lebanon from 1969 to 1982. Although the emphasis of his paper is thoracic vascular wounds, 1008 of his patients had peripheral vascular injuries or junctional hemorrhage.
Typical wounding mechanisms during that time in Lebanon were AK and M16 rifles, as well as rockets, and explosives. Sixty-three percent of his patients were military and 37% were civilian. During the time of that conflict, body armor would have been sparse at best. If armor was available, it would have been more traditional military “flak vests,” which have limited ballistic protection as they were designed to stop larger, high velocity, non-aerodynamic metal fragments, not bullets. Certainly, we can assume the 37% of his patients that were civilian were un-armored.

Of the Lebanese surgeon’s 1008 casualties with peripheral vascular injuries, 50% involved femoral and popliteal vasculature which we would assume could be managed with a tourniquet.
However, adding together injury to a “junctional” artery, vein, or both, 5% of patients had subclavian, 2% axillary, and 10% iliac vessel injuries. Carotid artery and Jugular vein injuries accounted for another 10% of injuries. Therefore 27% of his patients with what he felt were peripheral vascular injuries would not be expected to be manageable with a tourniquet. Although there are four “Junctional Tourniquets” commercially available, their penetrance in the civilian US market is minimal.
What does all this mean? You need to know how to pack junctional wounds if you are to save a casualty from bleeding to death from wounds in these locations. You can learn these skills in our online classes.
Preview CourseNot sure? Try a preview TRAIN NOWOnline Tactical Casualty Care Classes
References:
*1 J Trauma Acute Care Surg. 2012 Dec;73(6 Suppl 5):S431-7. Death on the battlefield (2001-2011): implications for the future of combat casualty care. Eastridge BJ
*2 J Thorac Cardiovasc Surg. 1985 May;89(5):723-33. Cardiovascular and thoracic battle injuries in the Lebanon War. Analysis of 3,000 personal cases. Zakharia AT.