🕖 Reading Time, 3 minutes
One of the best parts of the Special Operations Medical Association annual meeting is connecting with your peers and discussing issues we all deal with.
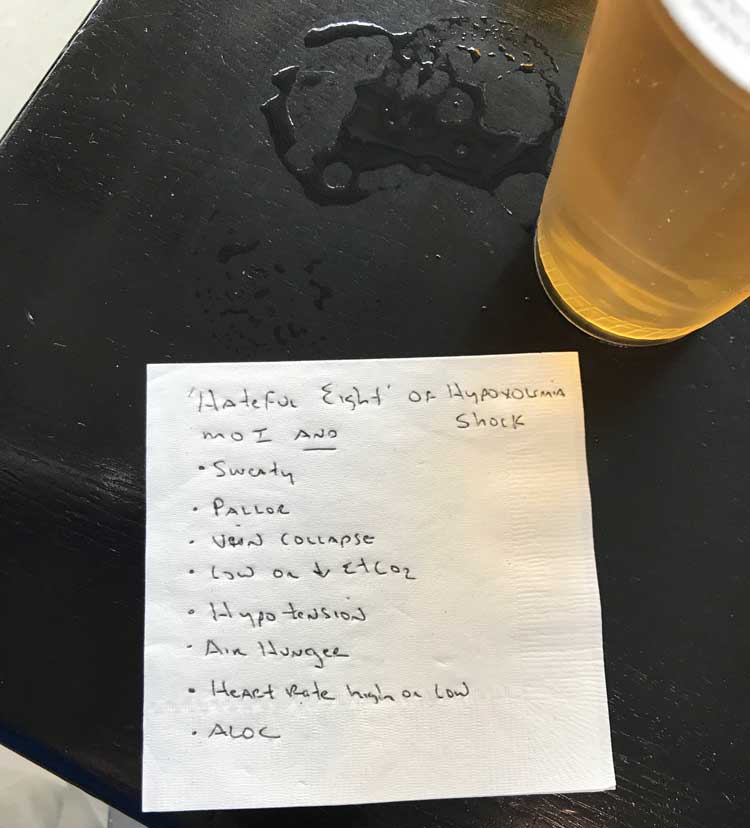
One evening, while having a bar napkin discussion about prehospital blood product administration, a London HEMS anesthetist and I discussed a teaching model one of her colleagues uses to help identify patients who are in shock from blood-loss and might benefit from blood administration. Obviously, giving blood to a patient in cardiogenic shock from massive AMI (heart attack) won’t help and might make things worse. They have heart pump failure, not blood volume loss.
If you think someone is in shock from blood loss, they need a mechanism of injury (MOI) that would cause blood loss, i.e., trauma, GSW, stabbing, and several of the “hateful eight,” before administering prehospital blood.
The Hateful Eight:
- Sweaty
- Pallor (because it’s the UK, the Americans would say “pale”)
- Collapsed veins
- Low or falling end-tidal CO2
- Hypotension
- Air hunger
- Abnormal heart rate, either high or low
- Altered mental status
As an example of how this model helps: Patients in shock from any cause could be sweaty, but acute blood volume loss can make your veins flat or collapsed as opposed to cardiogenic shock, where veins tend to be plump and more full as you have enough blood it just isn’t being pumped well. That would similarly apply to obstructive shock from tension pneumothorax or pericardial tamponade.
Keeping the hateful eight in mind before administering blood to a casualty in shock just might save you from going down the wrong path and causing the patient a new problem which you will then have to fix.