Pediatric Needle Decompression: Are We Using the Right Site and Needle Length?
- Posted by Mike Shertz MD/18D
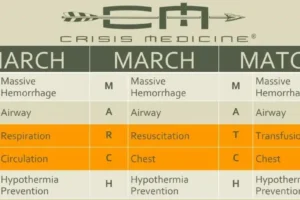
- Categories (R) Respiration, MARCH
Researched and written by Mike Shertz, MD/18D, not AI
Pediatric-specific needle decompression recommendations remain an evolving discussion
🕖 Reading Time, 4 minutes
While adult guidelines for needle decompression for tension pneumothorax are well established, pediatric-specific recommendations remain an evolving discussion. Recent studies using CT and ultrasound have refined our understanding of pediatric chest wall thickness and the depth to vital structures
Understanding Pediatric Chest Wall Thickness
A retrospective study of 250 children under 13 years old undergoing chest CT measured chest wall thickness (CWT) at two key locations: the 2nd intercostal space (ICS), mid-clavicular line (MCL), and the 4th ICS, anterior axillary line (AAL).
2nd ICS MCL: CWT ranged from 1.6 to 2.5 cm, with a 95th percentile thickness of 3.8 cm.
4th ICS AAL: CWT ranged from 1.6 to 2.2 cm, with a 95th percentile thickness of 4.2 cm.
Based on these measurements, the authors concluded that a 1.5-inch (3.8 cm) 14 or 16 gauge IV catheter is an appropriate choice for pediatric needle decompression.1
However, some authors have also questioned the generalizability of CT chest data as most children don’t undergo CT imaging with its substantial radiation exposure. Additionally, for optimal CT imaging, children are placed with their arms up over their heads, which might reduce the thickness of their anterior chest wall because of the extension of the pectoralis major musculature in this position.

Ultrasound Data: A Radiation-Free Alternative
Ultrasound doesn’t pose a radiation exposure risk, nor require the “arm up positioning.” A convenience sample of 163 children, aged 0 to 16 years old, undergoing point of care ultrasound had the thickness of their chest walls measured at the 2nd intercostal space (ICS) mid clavicular line (MCL) and 4th ICS anterior axillae line (AAL)
In children weighing 3–5 kg, mean CWT was 1.11 cm (2nd ICS MCL) and 1.13 cm (4th ICS AAL).
In children over 36 kg, mean CWT was 2.36 cm (2nd ICS MCL) and 2.58 cm (4th ICS AAL).
This continues to support the recommendation for a 1.5 inch (3.8cm) 14 or 16 gauge IV catheter as an appropriate size for needle decompression in pediatrics.2
…Now that we’ve gotten some consensus on pediatric chest wall thickness, how close inside the child’s chest are important structures we don’t want to hit with a needle?
How Close Are Vital Structures?
A convenience sample of 139 children, aged 10 years old and under undergoing chest CT, had the thickness of their chest walls measured at the 2nd intercostal space (ICS) mid clavicular line (MCL) and 4th ICS anterior axillae line (AAL) and also the depth to vital structures (DVS) within the chest at those locations. Vital structures were defined as the pericardium, aorta, superior vena cava, inferior vena cava, thymus gland, and pulmonary vessels segmental or larger.

Depth to Vital Structures by Age Group with correct needle decompression technique:
Newborns (0 years old):
2nd ICS MCL: 4.9 cm,
4th ICS AAL (left): 3.15 cm
5-year-olds:
2nd ICS MCL: 6.8 cm
4th ICS AAL (left): 4.3 cm
10-year-olds:
2nd ICS MCL: 9.2 cm
4th ICS AAL (left): 6.11 cm
Importantly, when improper technique was simulated (i.e., directing the needle toward a vital structure), the DVS was significantly smaller across all age groups and locations.
Notably, the thymus and heart were directly adjacent to the chest wall at the 2nd ICS MCL in several children aged 0 and 5 years. As a result, the study authors recommended the 4th ICS AAL as the preferred site for pediatric needle decompression. However, they also found that the DVS at the 4th ICS AAL was generally shorter, particularly on the left side, requiring careful technique.3
…We’ve worked out chest wall thickness in pediatric patients, understand what sites to use to maximize not hitting vital structures, but how effective is needle decompression in children?
Real-World Outcomes: Does Needle Decompression Work in Kids?
10 children received prehospital needle decompression at the 2nd ICS MCL before chest tube placement.
6 of the ten failed to improve clinically after the procedure. The remaining four improved, but deteriorated with recurrent “tension physiology.”
8 of 14 underwent prehospital paramedic thoracostomy.
This data highlights the high failure rate of needle decompression in children at the traditional 2nd ICS MCL site, reinforcing the need for careful site selection and possibly a shift toward 4th ICS AAL placement.
Conclusion
This research provides clarification into pediatric chest wall thickness, depth to vital structures, and raises questions of the effectiveness of needle decompression in pediatrics.
A 1.5-inch (3.8 cm) catheter remains appropriate for most pediatric patients.
The 4th ICS AAL is likely the safer insertion site, especially in younger children, to avoid the heart and thymus.
Needle decompression at the 2nd ICS MCL had a high failure rate in a single center study.
As more evidence emerges, pediatric needle decompression protocols should continue to evolve to maximize safety and efficacy in the field.
References
1Mandt MJ, Hayes K, Severyn F, Adelgais K. Appropriate Needle Length for Emergent Pediatric Needle Thoracostomy Utilizing Computed Tomography. Prehosp Emerg Care. 2019 Sep-Oct;23(5):663-671. doi: 10.1080/10903127.2019.1566422. Epub 2019 Feb 4. PMID: 30624127.
2Hossain R, Qadri U, Dembowski N, Garcia A, Chen L, Cicero MX, Riera A. Sound and Air: Ultrasonographic Measurements of Pediatric Chest Wall Thickness and Implications for Needle Decompression of Tension Pneumothorax. Pediatr Emerg Care. 2021 Dec 1;37(12):e1544-e1548. doi: 10.1097/PEC.0000000000002112. PMID: 32925707.
3Terboven T, Leonhard G, Wessel L, Viergutz T, Rudolph M, Schöler M, Weis M, Haubenreisser H. Chest wall thickness and depth to vital structures in paediatric patients – implications for prehospital needle decompression of tension pneumothorax. Scand J Trauma Resusc Emerg Med. 2019 Apr 16;27(1):45. doi: 10.1186/s13049-019-0623-5. PMID: 30992028; PMCID: PMC6469218.
4Quinn N, Palmer CS, Bernard S, Noonan M, Teague WJ. Thoracostomy in children with severe trauma: An overview of the paediatric experience in Victoria, Australia. Emerg Med Australas. 2020 Feb;32(1):117-126. doi: 10
Dr. Mike Shertz is the Owner and Lead Instructor at Crisis Medicine. Dr. Shertz is a dual-boarded Emergency Medicine and EMS physician, having spent over 30 years gaining the experience and insight to create and provide his comprehensive, science-informed, training to better prepare everyday citizens, law enforcement, EMS, and the military to manage casualties and wounded in high-risk environments. Drawing on his prior experience as an Army Special Forces medic (18D), two decades as an armed, embedded tactical medic on a regional SWAT team, and as a Fire Service and EMS medical director.
Using a combination of current and historical events, Dr. Shertz’s lectures include relevant, illustrative photos, as well as hands-on demonstrations to demystify the how, why, when to use each emergency medical procedure you need to become a Force Multiplier for Good.