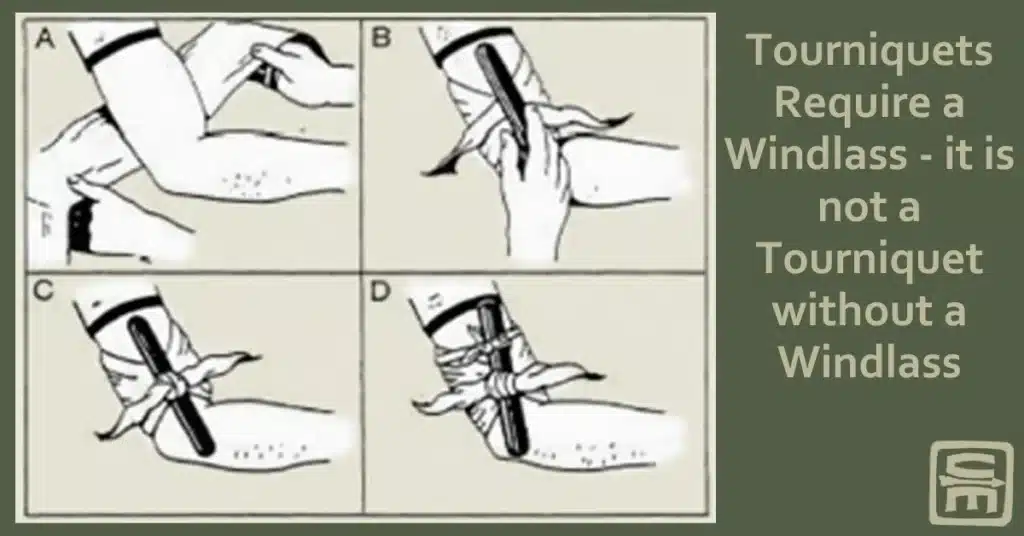
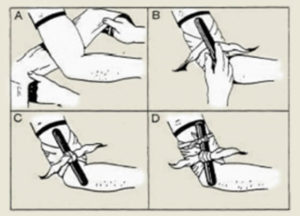
Tourniquets Require a Windlass
It is not a tourniquet if if does not have a windlass.
🕖 Reading Time, 7 minutes
Recent news articles describe many cases of the public placing “tourniquets” without windlasses on injured individuals to stop bleeding. However, if you look a little deeper, most of those well-intentioned “tourniquet” applications weren’t actually tourniquets at all and may endanger lives by increasing bleeding.
A tourniquet is a constricting band placed around a limb and tightened to eliminate arterial flow past the device. Simply tying a constricting band tightly around a limb rarely provides enough pressure to occlude arterial flow. To stop bleeding requires a mechanical advantage, and to obtain that advantage you need a windlass or twist stick to tighten the constricting material.
Arterial flow into the limb is a high-pressure system and requires high pressure deep in the limb to occlude or stop its flow. Venous flow is a low-pressure system taking blood from the limb and returning it back to the body and requires less pressure to stop its progress.
Material wrapped tightly around a limb, but without a “twist stick” for mechanical advantage is a venous constricting band at best. Although arterial flow is still present, moving blood into the injured limb, the venous system is occluded and can’t return blood to the body. So where will that blood go? Out of the wound and out of the body. When you have blood drawn at the doctor, the phlebotomist places a “venous constricting band” around your arm to occlude your venous system which engorges your veins, making it easier to draw blood from your enlarged veins.
Representative Examples of tourniquets without windlasses
For example, as mentioned previously in the post on tourniquets and children, a 7-year-old boy was struck in the leg by a piece of metal flung from a running lawnmower. The metal lacerated his femoral artery and broke his femur. Before the arrival of EMS, a rag was tied around the child’s leg proximal (between the injury and torso) to the wound. The child was in shock from his blood loss and EMS noted “slow,” but active continued bleeding from the wound, meaning the rag did not stop all blood flow as a tourniquet is designed to do.

There are several reports of girls using handbag straps wrapped around their legs to “stem” the bleeding after the Manchester bombing. Although it’s phenomenal that these young girls, most of whom likely had no formal medical training, made a management plan and carried it out in a very extreme situation, it is unlikely they used a windlass or twist stick to generate the pressure necessary to eliminate arterial flow past the strap.
Similarly, an article looking at tourniquet uses at the Boston Marathon bombing described the bombing as “the first major, modern US terrorist event with multiple, severe, warlike, lower extremity injuries.” They evaluated 66 patients with extremity injuries from the blast:
- 29 (44%) of the casualties had documented life-threatening hemorrhage at the point of injury (POI).
- 15 casualties had at least one lower extremity amputation
- Of the 29 casualties with life-threatening hemorrhage, 27 “improvised tourniquets” were placed at the POI.
- 16 casualties with a lower extremity amputation all had “improvised tourniquets,” including those placed by Boston EMS (who were not carrying commercially available tourniquets at that time).
- Overall, non-EMS responders placed 67% of the tourniquets.
At one receiving hospital, six casualties all had “improvised tourniquets” placed without a windlass and thus were “venous constricting bands.” All had to be replaced with commercial tourniquets to prevent ongoing hemorrhage.

Overall, many improvised tourniquets were documented to be “venous constricting bands” with “paradoxical (unexplained) bleeding” at time of evaluation in the Emergency Department.
Improvised tourniquets can work when applied properly.
An improvised tourniquet should be wide enough (2 to 3 inches) to compress both arteries and veins within the limb and have a device attached to generate the mechanical advantage necessary to cause circumferential limb constriction, with a goal to stop all blood flow.
This mistake is how you turn a non-life-threatening injury into a fatal one. What was noted at Boston as “paradoxical bleeding” from the “improvised tourniquets” and quite possibly the 7-year-old with “slow” bleeding was likely the result of a venous constricting band and was, in fact, increasing the blood loss to the casualties.
“Tourniquets” without windlasses are venous constricting bands
In a study using a large men’s cotton t-shirt wrapped tightly around the thigh of a computerized tourniquet trainer, the windlass lacking t-shirt “improvised tourniquet” failed to generate enough pressure to stop the computerized bleeding in 79 out of 80 attempts. Although it generated 46 mmHg pressure on the limb, this is not nearly enough for arterial occlusion but is more than enough for venous constriction. Venous constriction actually increases blood loss from an otherwise minimally bleeding wound.
Windlasses can be improvised too
The same t-shirt with a windlass made from chopsticks stopped the computerized model from bleeding in 54 of 80 attempts. Although far from 100% effective, 68% effectiveness is substantially better than doing nothing when lacking the ideal or dedicated equipment.
The actual effectiveness of this improvised tourniquet made of a t-shirt and chopsticks is likely much higher as one of the two testers routinely stopped twisting the windlass if he saw tearing and skin pinching of the silicone thigh skin under the tightening windlass, fearing it would be too painful for the casualty to endure. The other tester didn’t stop at these inconsequential side effects, focusing instead on the massive hemorrhage, and continued twisting the windlass until the bleeding was stopped. Typically that tester generated 145 mmHg pressure on the limb.
Tourniquets hurt considerably less than bleeding to death.
Having placed hundreds of similar improvised tourniquets on students, both adults and Girl Scouts of various ages, as well as myself, pinching of skin under the windlass occurs almost 100% of the time. However, even children can typically put up with it if you pull the windlass off the body just a bit when tightening.
One author studying improvised tourniquets said “… regarding tourniquets, the word pain becomes a criterion for tourniquet use, success, or failure. This is a tragic mistake and pain should be removed from the lexicon of tourniquet use. This symptom should be irrelevant.” The pain of a tourniquet is particularly irrelevant when its purpose is to stop a life-threatening hemorrhage.
Material tightly wrapped directly over the wound might be a “pressure dressing.” Even if placed proximally, it is very unlikely to ever become a tourniquet without a windlass to twist and tighten the material enough to constrict arterial flow. A “venous constricting band” is not a tourniquet, but rather a blood-letting device that increases hemorrhage and puts casualties at additional risk.
The media and the public need to understand this concept, stop calling a material wrapped tightly around a limb a tourniquet unless it has a windlass to generate the necessary mechanical advantage. Moreover, more people need to obtain training to truly assist in these life-threatening situations to stop preventable deaths from massive hemorrhage.
TRAIN NOWOnline Tactical Casualty Care Classes