Hypertonic Saline vs. Mannitol: What to Know About Severe TBI Treatment
- Posted by Mike Shertz MD/18D
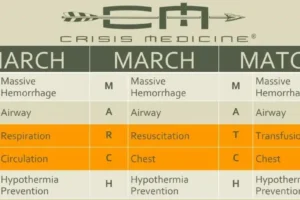
- Categories MARCH
National and international guidelines on TBI management don’t typically specify using mannitol or hypertonic saline, because there was never good data showing one was superior to the other. That may have changed.
Traumatic brain injuries (TBI) are a significant cause of morbidity and death. Increased intracranial pressure (ICP), an abnormally high pressure inside the skull associated with moderate to severe TBI, increases brain swelling or edema, increasing the likelihood of long-term impaired function and death.
Subsequently, controlling intracranial pressure is an important aspect of TBI management. This is often done by the administration of either mannitol or hypertonic saline. Mannitol is an osmotic diuretic, which pulls fluid out of the brain, eliminates it through urination, but can cause hypovolemia. In contrast, hypertonic saline pulls fluid out of the brain to “dilute” the high sodium levels in the blood.
Mannitol has a long history of use for treatment of elevated intracranial pressure. It has been used for so long that it precedes the more rigorous modern drug approval process now required by the FDA to show a new drug is effective.1
Typically, both national and international guidelines on TBI management don’t specify one drug over the other, because there was never good data showing one was superior to the other.1
In 2021, a systematic review and meta-analysis of the existing literature looking at those two treatments for severe TBI was published. Twelve randomized controlled trials across 464 patients showed no statistically significant survival or favorable neurological outcome with one drug or the other. This was consistent with multiple prior studies finding similar non-significant differences between the two treatments. Although in the systematic review and meta-analysis there was a trend toward improved survival with hypertonic saline, it just didn’t reach a statistically significant number.1

Administration of mannitol, because it is a diuretic, can cause decreased blood pressure and hypotension. We know from a prior landmark study on TBI2, that any hypotension (systolic blood pressure less than 90 mmHg) after significant head injury increases the casualty’s chance of dying by 2.5 times. Hypertonic saline has a theoretical advantage as it has previously been used for small volume resuscitation. It also has a longer duration of effect which might account for its improved 60-to-120-minute improved ICP.
One shortcoming with all the previous data is it hasn’t looked at the treatment effects of these drugs if they are administered before arrival to the hospital.
Enter a study comparing 20% mannitol to 20% hypertonic saline, administered prehospital, in moderate to severe TBI patients with pupillary dilation (suggestive of impending brain herniation, need for neurosurgical intervention, and death). This retrospective cohort study used data from 2011 to 2021, across 23 French trauma centers looking at 1417 patients aged 16 or over. Those receiving hypertonic saline had a 9% higher ICU survival (54% vs. 45%). Because of the data they had, they couldn’t comment on overall survival or neurological outcome. This is the largest study to date.3
Putting all of this together, moderate to severe TBI patients, particularly with pupil dilation have a high fatality rate and poor neurological outcome even if they survive. These patients need emergent brain imaging and neurosurgical consultation. If ICP lowering medications are used, hypertonic saline seems a better choice over mannitol, with its trend to higher overall survival, longer duration of effect, beneficial effects on hemodynamics, ability to lower increased ICP after mannitol failed to do so, and 9% higher ICU survival when administered prehospital.
Granted, the trend to higher overall survival didn’t reach a statistically significant value and surviving the ICU only to die on a hospital ward isn’t truly surviving, but the casualty has to get out of the ICU if they are to survive at all.
References:
1Schwimmbeck F, Voellger B, Chappell D, Eberhart L. Hypertonic Saline Versus Mannitol for Traumatic Brain Injury: A Systematic Review and Meta-analysis With Trial Sequential Analysis. J Neurosurg Anesthesiol. 2021 Jan;33(1):10-20. doi: 10.1097/ANA.0000000000000644. PMID: 31567726.
2Spaite DW, Hu C, Bobrow BJ, Chikani V, Barnhart B, Gaither JB, Denninghoff KR, Adelson PD, Keim SM, Viscusi C, Mullins T, Sherrill D. The Effect of Combined Out-of-Hospital Hypotension and Hypoxia on Mortality in Major Traumatic Brain Injury. Ann Emerg Med. 2017 Jan;69(1):62-72. doi: 10.1016/j.annemergmed.2016.08.007. Epub 2016 Sep 28. PMID: 27692683; PMCID: PMC5173421.
3Codorniu A, Charbit E, Werner M, James A, Hanouz JL, Jost D, Severin A, Lang E, Pottecher J, Favreau M, Weiss E, Abback PS, Moyer JD; TraumaBase Group. Comparison of mannitol and hypertonic saline solution for the treatment of suspected brain herniation during prehospital management of traumatic brain injury patients. Eur J Emerg Med. 2024 Aug 1;31(4):287-293. doi: 10.1097/MEJ.0000000000001138. Epub 2024 Apr 30. PMID: 38691014.
Dr. Mike Shertz is the Owner and Lead Instructor at Crisis Medicine. Dr. Shertz is a dual-boarded Emergency Medicine and EMS physician, having spent over 30 years gaining the experience and insight to create and provide his comprehensive, science-informed, training to better prepare everyday citizens, law enforcement, EMS, and the military to manage casualties and wounded in high-risk environments. Drawing on his prior experience as an Army Special Forces medic (18D), two decades as an armed, embedded tactical medic on a regional SWAT team, and as a Fire Service and EMS medical director.
Using a combination of current and historical events, Dr. Shertz’s lectures include relevant, illustrative photos, as well as hands-on demonstrations to demystify the how, why, when to use each emergency medical procedure you need to become a Force Multiplier for Good.