What can we learn from case reports of NPAs gone wrong
- Posted by Mike Shertz MD/18D
- Categories (A) Airway
🕖 Reading Time, 6 minutes
There has been recent discussion about the rarity of significant complications from nasopharyngeal airway (NPA) placement. Many chalk the cases of inadvertent intracranial placement as essentially “something that never happens.”
We were asked by a student: “Exactly how often does inadvertent placement of an NPA into the brain occur?” The published English language medical literature describes five cases across several decades.
Is there anything to be learned from those five cases and do they have anything in common or an actual teaching point?
Limitations on NPA Use
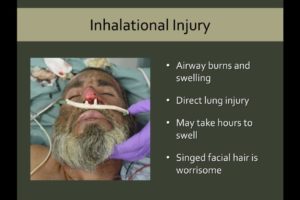
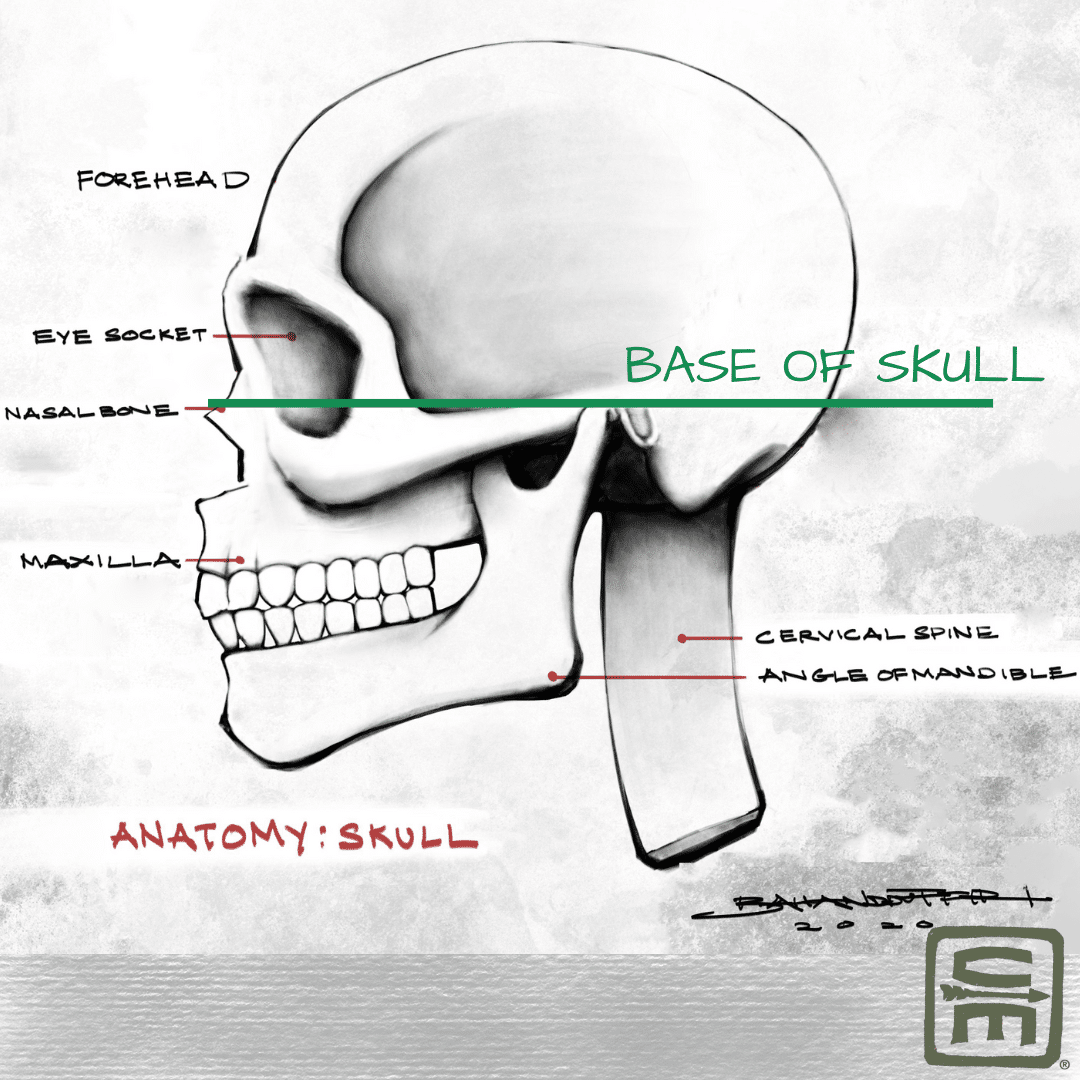
It is often said nasal pharyngeal airways shouldn’t be placed if the casualty has a “bloody face.” The issue is a concern the NPA might track into the casualty’s brain through a facial / skull fracture, rather than properly along the nasal floor with the tip ending just above the epiglottis. With facial fractures, the possibility of misplacement exists, but the concern is largely if the casualty has a basal skull fracture, which can be very difficult to diagnose clinically.
Published Cases
Published case reports are often described as something that happened once (so it’s interesting to publish) but will likely never happen again. Once several case reports of an event are published, there is a bias not to report additional cases because it has “been described already.” Misplacement of an NPA into the brain might occur more frequently than those five events; it’s difficult to say.
1
The first reported case of an NPA, placed nasally, entering the cranial vault was in 1991. A 46-year-old female was involved in an MVC and sustained multiple facial fractures, basal skull fracture, frontoparietal skull fractures, and facial edema. Before ED arrival, she developed respiratory depression, and an NPA was placed. CT scan of her brain, after ED intubation, showed intracranial placement.1
2
The second case report was in 1999. A 29-year-old male was crushed between two tractor cabs. He had severe facial fractures, facial bleeding, and was responsive largely only to pain. After several unsuccessful attempts at oral intubation, an NPA was placed. During transport, it was reported as visible several times in the oropharynx. CT imaging in the ED confirmed multiple facial and basal skull fractures, as well as the tip of the NPA in the brain. There was speculation that the NPA became mispositioned and penetrated the cranial vault because of patient handling and movement. The authors noted that the rubber, plastic, or silastic materials the devices are made of become more flexible as they warm to body temperature which could allow them to follow fracture contours resulting in misplacement.2
3
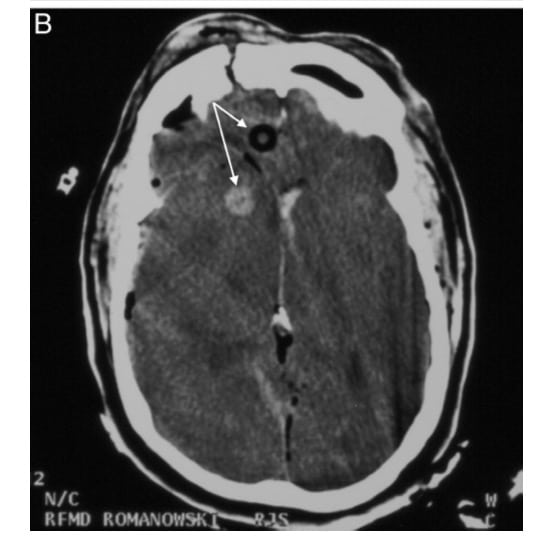
The third case was a 43-year-old male thrown head-first into a guardrail after a motorcycle accident. He had severe craniofacial injuries. Intubation was deferred prehospital secondary to concerns for severe facial trauma and C-spine immobilization. Instead, bilateral NPAs were placed. If the face is too damaged for endotracheal intubation, NPA placement is clearly contraindicated. Ultimately, his CT imaging showed comminuted anterior skull base fractures and intercranial placement of an NPA.5 (See the CT from this case below).
4
The fourth case was published in 2006. An adult cab driver involved in a head on collision had significant facial trauma. Paramedics couldn’t open his mouth, were concerned about his airway, and inserted an NPA. CT imaging showed multiple facial fractures, including his basal skull, and the NPA tip in the cab driver’s brain.4
5
Many argue about the overall effectiveness of the NPA as an airway adjunct. Personally, I have had great luck with them. Many casualties don’t necessarily need NPA placement to maintain their airway if they can be rolled into the recovery position. If they can’t, and no one is available to constantly maintain a head tilt / chin lift position on the casualty, the NPA can often suffice to keep the airway open.
Is fear of placing an NPA into a “bloody face” warranted? Yes and no.
Four of five case reports are of casualties with blunt facial trauma, significant facial fractures, and facial edema. If the casualty has mid facial trauma / swelling and you’re concerned for facial fractures or basal skull fracture, the NPA is best avoided so you don’t become case report number six, and somebody has to remove the NPA tip from the casualty’s brain.
In the sole casualty with a head GSW and an obstructed airway, predicting the cribriform plate damage would have been difficult. If there isn’t much facial trauma, the facial anatomy looks intact, and you don’t have a better way to maintain the casualty’s airway, placement of the NPA still seems reasonable.
References
1Muzzi DA, Losasso TJ, Cucchiara RF. Complication from a nasopharyngeal airway in a patient with a basilar skull fracture. Anesthesiology. 1991 Feb;74(2):366-8. doi: 10.1097/00000542-199102000-00026. PMID: 1990912.
2Schade K, Borzotta A, Michaels A. Intracranial malposition of nasopharyngeal airway. J Trauma. 2000 Nov;49(5):967-8. doi: 10.1097/00005373-200011000-00032. PMID: 11086797.
3Roberts K, Whalley H, Bleetman A. The nasopharyngeal airway: dispelling myths and establishing the facts. Emerg Med J. 2005 Jun;22(6):394-6. doi: 10.1136/emj.2004.021402. PMID: 15911941; PMCID: PMC1726817.
4Ellis DY, Lambert C, Shirley P. Intracranial placement of nasopharyngeal airways: is it all that rare? Emerg Med J. 2006 Aug;23(8):661. doi: 10.1136/emj.2006.036541. PMID: 16858116; PMCID: PMC2564185.
5Martin JE, Mehta R, Aarabi B, Ecklund JE, Martin AH, Ling GS. Intracranial insertion of a nasopharyngeal airway in a patient with craniofacial trauma. Mil Med. 2004 Jun;169(6):496-7. doi: 10.7205/milmed.169.6.496. PMID: 15281683.
6Steinbruner D, Mazur R, Mahoney PF. Intracranial placement of a nasopharyngeal airway in a gun shot victim. Emerg Med J. 2007 Apr;24(4):311. doi: 10.1136/emj.2007.046490. PMID: 17384400; PMCID: PMC2658253.
Dr. Mike Shertz is the Owner and Lead Instructor at Crisis Medicine. Dr. Shertz is a dual-boarded Emergency Medicine and EMS physician, having spent over 30 years gaining the experience and insight to create and provide his comprehensive, science-informed, training to better prepare everyday citizens, law enforcement, EMS, and the military to manage casualties and wounded in high-risk environments. Drawing on his prior experience as an Army Special Forces medic (18D), two decades as an armed, embedded tactical medic on a regional SWAT team, and as a Fire Service and EMS medical director.
Using a combination of current and historical events, Dr. Shertz’s lectures include relevant, illustrative photos, as well as hands-on demonstrations to demystify the how, why, when to use each emergency medical procedure you need to become a Force Multiplier for Good.